Welcome To The Dry Eye Center at Eyesymmetry Vision Center Dry Eye Center In Baltimore, MD
Even without knowing the term “dry eye” or “Dry Eye Syndrome“, if you suffer from it, then you are all too familiar with the soreness, discomfort, and even the constant misery that can come with dry eyes.
Fortunately, there is a Dry Eye Specialist seeking to bring relief and healing from Dry Eyes in its many forms to patients from the state of Maryland. With Dr. Moshe Schwartz and Dr. Jenny Chen at the helm, the The Dry Eye Center at Eyesymmetry Vision Center specializes in treating the entire range of Dry Eye Syndrome, from mild to severe. Whether it’s an occasional irritant or a debilitating daily problem, we’re here to help, with years of experience specializing in treating dry eyes.
The The Dry Eye Center at Eyesymmetry Vision Center uses the most advanced diagnostic equipment and tools to quickly and accurately pinpoint the cause and type of dry eye problem you’re suffering from. We don’t just throw any old drops at you either. We provide custom, tailored treatment plans designed to maximize the relief of your dry eye symptoms AND treat the underlying cause of your discomfort.

Dry Eye Treatment In Baltimore
Even without knowing the term “dry eye” or “Dry Eye Syndrome“, if you suffer from it, then you are all too familiar with the soreness, discomfort, and sometimes even the constant misery that can come with dry eyes.
Fortunately, there is a Dry Eye Specialist seeking to bring relief and healing from Dry Eyes in its many forms to patients from the state of Maryland. With Dr. Moshe Schwartz and Dr. Jenny Chen at the helm, the The Dry Eye Center at Eyesymmetry Vision Center specializes in treating the gamut of dry eyes. Whether it’s an occasional irritant or a debilitating daily problem, we’re here to help, with years of experience specializing in treating dry eyes.
The The Dry Eye Center at Eyesymmetry Vision Center uses the most advanced diagnostic equipment and tools to quickly and accurately pinpoint the cause and type of dry eye problem you’re suffering from. We don’t just throw any old drops at you either. We provide custom, tailored treatment plans designed to maximize the relief of your dry eye symptoms AND treat the underlying cause of your discomfort.

Dry Eye Syndrome can range from a mild irritant to chronic problem. The symptoms of Dry Eye Syndrome may include:
- Dry, irritated, or red eyes
- Excessive tearing/watery eyes
- Inflammation
- Sore or sensitive eyes
- Itchiness
- Burning or inflammation
- A gritty or pasty feeling in the eyelids
- Crusty or gunky eyes
- Blurriness

Dry Eye Syndrome can range from a mild irritant to chronic problem. The symptoms of Dry Eye Syndrome may include:
-
- Dry, irritated, or red eyes
- Excessive tearing/watery eyes
- Inflammation
- Sore or sensitive eyes
- Itchiness
- Burning or inflammation
- A gritty or pasty feeling in the eyelids
- Crusty or gunky eyes
- Blurriness



As we age, we experience hormonal changes. These changes are known to cause or contribute to dry eyes. While this is true of both men and women, it seems that women over 50 are particularly more prone to developing dry eye symptoms. Pregnancy is also known to contribute to or exacerbate dry eye syndrome.
By increasing the rate at which our tears evaporate, the following environmental factors are known to play a huge role in causing or contributing to dry eyes:
- Smoke
- Allergens
- Pollution
- Cold-climate and central heating
- Dry climate
- Sandy or dusty conditions
- Altitude
Poor cleaning habits, not changing the contact often enough, and sleeping in contact lenses can all contribute to dry eyes. However, even for those who take proper care with their contacts, they can still be a contributing cause of dry eyes. In fact, one of the main reasons people discontinue contact lens usage is due to dry eyes. The good news is there have been major improvements across all the brands with special contacts that are aimed at preventing dry eye symptoms.



Various diseases contribute to, or even cause, dry eyes. Autoimmune diseases are a known factor. Rheumatoid arthritis and Sjogren’s syndrome – a common symptom that rheumatologists treat can also contribute to dry eyes. Diabetics or those with Glaucoma that requires medication are also more likely to have dry eye syndrome.
As with everything, proper balanced diet and exercise are important in preventing or managing dry eye syndrome. There are two specific activities that relate directly to Dry Eyes.
Does Staring At A Screen Cause Dry Eye?
Continuous staring at a fixed object, such as a phone or computer screen, usually results in a decreased blink rate. The lack of blinking actually causes the eyes not to replenish the tears often enough. The meibomian glands, therefore, can become blocked or even atrophy and die.
Prolonged And Continuous Use Of Digital Devices Is Thought To Be The Likely Culprit In The Significant Increase Of Dry Eye Syndrome Throughout The General Population.
Does Drinking More Water Help With Dry Eye?
The main component of tears is water. Most of us don’t drink enough water. If you are dehydrated or not drinking enough, then you may not produce enough tears to keep your eyes moist. Snapple, Coke and other caffeinated drinks like coffee and tea may feel like they quench your thirst, but they actually dehydrate the body. Your body needs water to prevent dry eyes symptoms.
Whether prescription or over-the-counter, certain medications are known to decrease tear production or otherwise contribute to Dry Eye Syndrome. These include:
- Beta-blockers / blood pressure medications
- Antihistamines
- Decongestants
- AntiDepressants
- Oral Contraceptives

As we age, we experience hormonal changes. These changes are known to cause or contribute to dry eyes. While this is true of both men and women, it seems that women over 50 are particularly more prone to developing dry eye symptoms. Pregnancy is also known to contribute to or exacerbate dry eye syndrome.
By increasing the rate at which our tears evaporate, the following environmental factors are known to play a huge role in causing or contributing to dry eyes:
- Smoke
- Pollution
- Cold-climate and central heating
- Dry climate
- Sandy or dusty conditions
- Altitude
Poor cleaning habits, not changing the contact often enough, and sleeping in contact lenses can contribute to dry eyes. However, even for those who take proper care with their contacts, they can still be a contributing cause of dry eyes. In fact, one of the main reasons people discontinue contact lens usage is due to dry eyes. The good news is there have been major improvements across all the brands with special contacts that are aimed at preventing dry eye symptoms.
Various diseases contribute to, or even cause, dry eyes. Autoimmune diseases are a known factor. Rheumatoid arthritis and Sjogren’s syndrome – a common symptom that rheumatologists treat can also contribute to dry eyes. Diabetics or those with Glaucoma that requires medication are also more likely to have dry eye syndrome.
As with everything, proper balanced diet and exercise are important in preventing or managing dry eye syndrome. There are two specific activities that relate directly to Dry Eyes.
Does Staring At A Screen Cause Dry Eye?
Continuous staring at a fixed object, such as a phone or computer screen, usually results in a decreased blink rate. The lack of blinking actually causes the eyes not to replenish the tears often enough. The meibomian glands, therefore, can become blocked or even atrophy and die.
Prolonged And Continuous Use Of Digital Devices Is Thought To Be The Likely Culprit In The Significant Increase Of Dry Eye Syndrome Throughout The General Population.
Does Drinking More Water Help With Dry Eye?
The main component of tears is water. Most of us don’t drink enough water. If you are dehydrated or not drinking enough, then you may not produce enough tears to keep your eyes moist. Snapple, Coke and other caffeinated drinks like coffee and tea may feel like they quench your thirst, but they actually dehydrate the body. Your body needs water to prevent dry eyes symptoms.
Whether prescription or over-the-counter, certain medications are known to decrease tear productions, or otherwise, contribute to Dry Eye Syndrome. These include:
- Beta-blockers / blood pressure medications
- Antihistamines
- Decongestants
- AntiDepressants
- Oral Contraceptives
Our Dry Eye Specialist in provides cutting-edge treatment for dry eyes that's fully tailored to your specific situation. We diagnose and assess your eyes using the latest technology combined with good old-fashioned visual exams, questions, and all around great patient care that will get to the core cause of your condition. For example:
- How effectively are you blinking? How often?
- Are your tear ducts lined up properly?
- What’s the osmolarity of your tears?
- How fast do your tears break down?
- What is your tear volume?
- How well are your meibomian glands functioning? Are they blocked? Dirty? Infected?
Our dry eye doctor will also conduct an in-depth assessment of indicators for other diseases and health problems which might be contributing factors to your dry eyes. We then develop a personalized treatment plan based on what we find, and ongoing based on what's working for you.
On every patient questionnaire, we ask if you are suffering from any of the typical symptoms of dry eyes. Do your eyes feel gritty? Sore? Do you feel like something is in your eye or that you just don't seem to have any tears? If you report symptoms of dry eye, or appear to exhibit those symptoms, then we recommend beginning the dry eye exam process, which is quick, easy, and painless.
The first thing we want to check is the stability of the tear-film. We use TearLab to test the osmolarity of your tears― that is, the relative concentrations of salts, water, and lipids (fatty oils). These lipids are produced by the meibomian glands. Most cases of dry eyes occur where there is a problem with these glands. They could be blocked, atrophied, or otherwise damaged. If your tears evaporate too quickly (which causes burning), it's usually caused by a lack of these lipids.
A strong imbalance between the osmolarity of one eye vs. the other is a strong indication that someone has dry eye disease.
Depending on the results of the TearLab, our Dry Eye specialist will also want to see if the overall volume of tears could be the problem. In some cases, the meibomian glands are producing the lipids needed for lubrication, but there just isn't enough of the aqueous layer (this means tears) to spread it around effectively.
In order to test this, our optometrist will place a thin piece of red thread draped over the eyes for a few seconds in order to measure how wet the eye gets and comparing the differential between the eyes.




Another tool in the arsenal of our dry eyes experts is InflammaDry, a specialized diagnostic tool which measures whether or not a patient has elevated levels of MMP-9 in their tears from the inner lining of the lower eyelid. MMP-9 is a protein which indicates inflammation, which is fairly common for anyone suffering from dry eyes.
Our eye doctor will typically prescribe steroids in order to get the eye inflammation under control.
Sometimes, a visual inspection of the eyes isn't enough. Since a problem with the meibomian glands (which produce those essential lubricating lipids) is most often to blame for chronic dry eyes, it's important to get the best digital image of the meibomian glands possible. That's why our dry eye specialists use LipiScan, which takes a high-resolution digital image of the lower AND upper glands.
Such imaging tells us a lot about how healthy your oil glands are. Are they healthy? Blocked? Dilating? Atrophied? Gunky? Is the oil cloudy or clear? ― cloudy oil indicates the presence of a bacterial infection which thickens the oils until they simply are no longer effective. This we can usually clear up with antibiotics.
Our dry eye doctor will also test your tear breakup time. Sometimes, tears don't last long enough to work effectively. In order to test this, we use a fluorescein orange dye to test the breakup time (as well as any other corneal diseases, conditions, or foreign bodies). Using a small blotting paper, the optometrist will lightly touch your eye. As you blink, the dye spreads and gently coats the tear film covering the cornea. Using a blue light (the dye is orange), problems will be revealed to the eye doctor as green.

Our Dry Eye Specialist in provides cutting-edge treatment for dry eyes that's fully tailored to your specific situation. We diagnose and assess your eyes using the latest technology combined with good old-fashioned visual exams, questions, and all around great patient care that will get to the core cause of your condition. For example:
- How effectively are you blinking? How often?
- Are your tear ducts lined up properly?
- What’s the osmolarity of your tears?
- How fast do your tears break down?
- What is your tear volume?
- Do your tear ducts line up properly?
- What shape are your meibomian glands in? Are they blocked? Dirty? Infected?
Our dry eye doctor will also conduct an in-depth assessment of indicators for other diseases and health problems which might be contributing factors to your dry eyes. We then develop a personalized treatment plan based on what we find, and ongoing based on what's working for you.
On every patient questionnaire, we ask if you are suffering from any of the typical symptoms of dry eyes. Do your eyes feel gritty? Sore? Do you feel like something is in your eye or that you just don't seem to have any tears? If you report symptoms of dry eye, or appear to exhibit those symptoms, then we recommend beginning the dry eye exam process, which is quick, easy, and painless.
The first thing we want to check is the stability of the tear-film. We use TearLab to test the osmolarity of your tears― that is, the relative concentrations of salts, water, and lipids (fatty oils). These lipids are produced by the meibomian glands. Most cases of dry eyes occur where there is a problem with these glands. They could be blocked, atrophied, or otherwise damaged. If your tears evaporate too quickly (which causes burning), it's usually caused by a lack of these lipids.
A strong imbalance between the osmolarity of one eye vs. the other is a strong indication that someone has dry eye disease.
Depending on the results of the TearLab, our Dry Eye specialist will also want to see if the overall volume of tears could be the problem. In some cases, the meibomian glands are producing the lipids needed for lubrication, but there just isn't enough of the aqueous layer (this means tears) to spread it around effectively.
In order to test this, our optometrist will place a thin piece of red thread draped over the eyes for a few seconds in order to measure how wet the eye gets and comparing the differential between the eyes.
Another tool in the arsenal of our dry eyes experts is InflammaDry, a specialized diagnostic tool which measures whether or not a patient has elevated levels of MMP-9 in their tears from the inner lining of the lower eyelid. MMP-9 is a protein which indicates inflammation, which is fairly common for anyone suffering from dry eyes.
Our eye doctor will typically prescribe steroids in order to get the eye inflammation under control.
Sometimes, a visual inspection of the eyes isn't enough. Since a problem with the meibomian glands (which produce those essential lubricating lipids) is most often to blame for chronic dry eyes, it's important to get the best digital image of the meibomian glands possible. That's why our dry eye specialists use LipiScan, which takes a high-resolution digital image of the lower AND upper glands.
Such imaging tells us a lot about how healthy your oil glands are. Are they healthy? Blocked? Dilating? Atrophied? Gunky? Is the oil cloudy or clear? ― cloudy oil indicates the presence of a bacterial infection which thickens the oils until they simply are no longer effective. This we can usually clear up with antibiotics.
Our dry eye doctor will also test your tear breakup time. Sometimes, tears don't last long enough to work effectively. In order to test this, we use a fluorescein orange dye to test the breakup time (as well as any other corneal diseases, conditions, or foreign bodies). Using a small blotting paper, the optometrist will lightly touch your eye. As you blink, the dye spreads and gently coats the tear film covering the cornea. Using a blue light (the dye is orange), problems will be revealed to the eye doctor as green.

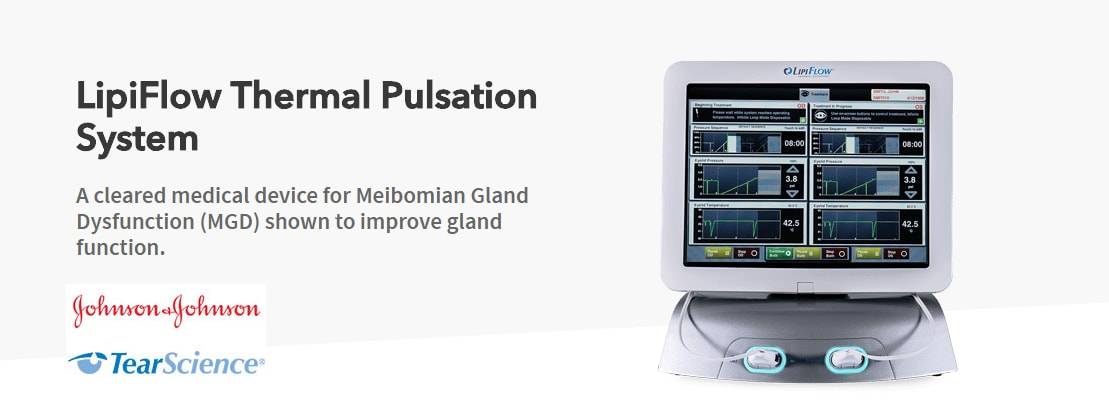
Lipiflow Treatment In Baltimore
85% of Dry Eye Syndrome is due to Meibomian Gland Disorder (MGD), where the glands essential for producing the lubricating oils for our eyes are blocked, clogged, dirty, infected, or atrophying.
Effectively treating MGD requires directly addressing the dysfunction in the meibomian glands. There are currently a number of treatments that attempt to stimulate the meibomian glands to produce more moisturizing and protective lipids. What LipiFlow does is directly massage and warm the meibomian glands in a safe, comfortable, and targeted way. LipiFlow is currently the only treatment which heats the meibomian glands directly from the undersurface of the upper and lower lids. LipiFlow uses vectored pulsation to simultaneously pump and express the blocked oil glands.
LipiFlow is the only electronic device to be FDA-approved for treating MGD. The procedure is backed up by significant research and clinical trials demonstrating that it is both safe and effective at treating chronic dry eyes and (MGD) Meibomian gland dysfunction.
Until the LipiFlow, treatment was mostly restricted to some combination of lubricating eye drops, hot compresses, and manual expression of the glands. In severe or chronic cases, these treatments are only rarely effective. What’s more, manual expression can be very painful and partially effective.
Instead of a combination of painful or partially effective treatments, LipiFlow both massages out blockages while simultaneously applying heat. The process uses”Vectored Thermal Pulsation Technology” ― A patented algorithm of precise heat is applied to the inner eyelids with directed gentle massage to remove blockages from the meibomian glands. This treatment is designed to restore the natural oil flow to the tear film that covers the eye’s surface